A Simple Test That Could Save The Lives Of Many Women In Nepal
In Nepal, researchers estimate that 2,244 women are diagnosed with cervical cancer every year and 1493 die from the disease.
Nepal has a cervical cancer incidence rate of 16.4 per 100,000 women, nearly four times the World Health Organisation (WHO) target of 4 per 100,000. So why is this preventable cancer ranked as the most common cancer among Nepali women?
Firstly, there is no national screening programme. Although the government and the Ministry of Health and Population issued national guidance on cancer screening and prevention in 2010, they substantially failed to meet their target goal of screening 70% of women in the age group of 30-60 years old by 2017 as only 8.2% of women aged 30-49 years were screened by 2019. Screening provides one of the most effective tools in preventing cervical cancer. In the UK, the NHS launched its cervical screening programme in 1988 and since the 1990’s cervical cancer incidence rates have decreased by 25%.
So what is cervical cancer screening and what are the barriers in Nepal? Could primary care infrastructure help?
What is Cervical Cancer Screening?
There are several different methods of screening. The most common method for cervical screening is the smear/pap test (Papanicolaou test). This is a test that is done to check the health of your cervix (the opening to your womb from the vagina) by taking a small sample of cells from the cervix with a soft brush. The test is conducted to help prevent cervical cancer; it is not a test for cancer. The other common type of screening is the HPV (Human Papilloma Virus) DNA test.
In the UK, national screening involves assessing whether patients are HPV positive – a known high-risk factor for developing cervical cancer. The sample for HPV DNA is taken via a small swab of the cervix. If HPV is negative, you will not need further action and will be followed up as per the screening programme. However, if you are HPV positive, it is crucial to assess the cervical cells for any detrimental changes that may lead to cancer or to identify cancerous cells. It is important to remember that if you are positive for HPV, it does not mean that you will definitely get cancer. Still, it means you will need to be monitored more carefully as you will be at a higher risk for cancer.
In Nepal, there is currently no national screening programme. Although the most common screening method is the Pap/Smear test, another common approach is the ‘see and treat approach’ which involves applying 3-5% acetic acid to the cervix. This will cause a colour change in abnormal cells, visible to the naked eye, allowing the doctor to identify women needing treatment. However, the major limitation of this approach is that it has lower sensitivity (lower ability to detect abnormal cervical cell changes) in women over 40 years old.
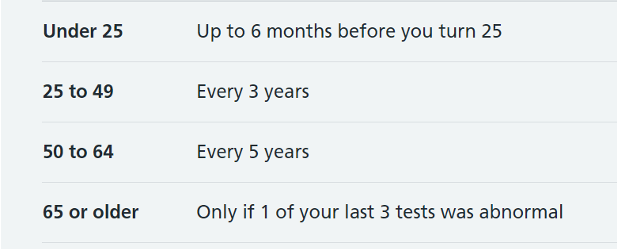
The current cervical screening programme in the UK
There are multiple reasons and factors that contribute to this low rate of cervical screening in Nepal. However, one key and pressing issue is the lack of healthcare infrastructure.
Barriers to Cervical Screening in Nepal
There are many barriers that developing countries like Nepal face when considering screening programmes. Firstly, there needs to be better healthcare infrastructure which would create consistency when providing services. With inconsistent services, it is difficult to provide and sustain essential healthcare messages such as disease prevention and the importance of screening. Further, given that the procedure is intimate, many women feel uncomfortable or embarrassed to go and see a doctor, thus creating another barrier to women coming forward and engaging in screening. Finally, the geographical terrain of Nepal means that healthcare is often centred in urban areas and cities, with rural communities often neglected and unable to access adequate healthcare without travelling to cities.
How Can Primary Care Infrastructure Help?
Nepal, like many other low and middle-income countries, has no primary healthcare infrastructure. In countries with established primary healthcare systems, healthcare professionals can regularly engage with members of their community and patients can build a therapeutic relationship with their primary care provider as it is their first point of contact for non-urgent care. This provides healthcare professionals such as doctors and nurses the opportunity to engage, educate and encourage patients to improve their health and well-being; for instance, providers can explain why cervical cancer screening is so important. Moreover, as patients are signed up to their primary care clinic, the clinic can send out reminders, monitor which patients are due for screening and provide compliance reminders if they have missed their screening appointment. As the clinic knows the patient and their health history, it provides the perfect opportunity to prevent disease, promote lifestyle changes and manage chronic diseases in the community.
In Nepal, patients are burdened with managing their own healthcare and entangled in a culture where they are often encouraged to ‘doctor shop’ and see multiple healthcare providers whom various friends and families have suggested. This creates a significant issue of patients receiving no continuity of care. Instead, they are given paper notes of their consultation which are easy misplace or lose. Subsequently, when consulting with another doctor, the physician is unaware of what has happened previously or the patient’s full medical history. This, combined with limited consultation time in a busy outpatient department, significantly impacts doctors’ ability to provide holistic healthcare. In contrast, primary healthcare offers a perfect platform to instigate preventative health measures such as screening programmes and can provide patients with the holistic care they need and deserve.
Looking Forward…
To implement a successful screening campaign, there needs to be a certain degree of health infrastructure and financial support to sustain it. This is likely the most significant limiting factor in instigating effective cervical screening in Nepal. National health promotion campaigns and patient education on cervical screening are essential to encourage women to seek medical attention to get their pap/smear tests. Unfortunately, without primary care, the burden is still placed on the patient to actively seek health prevention and screening tests. However, with national campaigns and education, patients are at least provided with the knowledge and tools to prevent disease.
The development of HPV DNA home testing kit has provided another effective clinical tool to save women’s lives. This self-testing kit involves women inserting a swab into their vagina and then sending the sample to the lab. It can be done by women at their convenience, at home. If the test is negative, then no further intervention is required. However, patients need to see their doctor if a positive result is demonstrated. In 2021, the WHO recommended DNA-based HPV testing as the first line for cervical cancer screening. Sweden has demonstrated great success using these kits and the WHO predicts that Sweden is on track to eliminate cervical cancer in the next five years. The home self-testing kits also provide an alternate avenue to reach more rural areas. Tests could be distributed in villages and marketplaces and returned on the same day for processing. This is cost-effective, not labour-intensive and provides women with privacy and the convenience of doing the test themselves.
For more informative articles and health tips, follow UpaCare Health and stay tuned for our blog!
References
IOC/IARC Information Centre on HPV and Cancer Nepal Human Papillomavirus and Related Cancers, Fact Sheet 2021 (2021)
Fang.C.Y et al. Overcoming Barriers to Cervical Cancer Screening Among Asian American Women, N Am J Med Sci (Boston). 2011; 4(2): 77–83.
Narasimhamurthy.M et Kafle. S.U, Cervical cancer in Nepal: Current screening strategies and challenges, Front. Public Health, 17 November 2022, Sec. Infectious Disease- Surveillance, Prevention and Treatment, Vol 10-2022.
HPV self-sampling in Sweden leading to faster elimination of cervical cancer, World Health Organisation (WHO) 2022.https://www.who.int/europe/news/item/08-09-2022-hpv-self-sampling-in-sweden-leading-to-faster-elimination-of-cervical-cancer.
Cervical screening: programme overview Information on the NHS Cervical Screening Programme, including commissioning, quality assurance, education, and training. Public Health England 2021, https://www.gov.uk/guidance/cervical-screening-programme-overview.